The lung volume reduction coil for the treatment of emphysema: a new therapy in development.
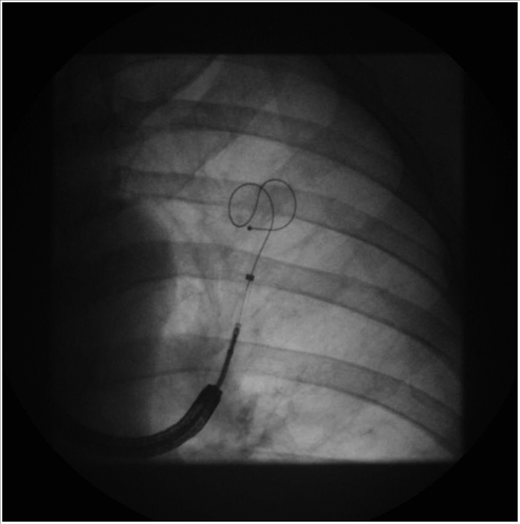 Lung volume reduction (LVR) coil treatment is a novel therapy for patients with severe emphysema. In this bilateral bronchoscopic treatment, approximately 10 LVR coils per lobe are delivered under fluoroscopic guidance in two sequential procedures.
Lung volume reduction (LVR) coil treatment is a novel therapy for patients with severe emphysema. In this bilateral bronchoscopic treatment, approximately 10 LVR coils per lobe are delivered under fluoroscopic guidance in two sequential procedures.
The LVR coil reduces lung volume by compressing the most destructed areas of the lung parenchyma and restores the lung elastic recoil. Both patients with upper- and lower-lobe predominant emphysema as well as a homogeneous emphysema distribution can be treated. LVR coil treatment results in an improvement of pulmonary function, exercise tolerance and quality of life. The LVR-coil treatment has been evaluated in several European clinical trials since 2008 and received CE mark approval in 2010.
Currently, two large multicenter randomized controlled trials are underway in Europe and North America to assess the efficacy and safety of the LVR-coil treatment at 12 months compared with usual care. In this review, we share our experience with the LVR-coil treatment.




 Surgical use of robots has evolved over the last 10 years. However, the academic experience with robotic lung segmentectomy remains limited. We aimed to analyze our lung segmentectomy experience with robot-assisted thoracoscopic surgery.
Surgical use of robots has evolved over the last 10 years. However, the academic experience with robotic lung segmentectomy remains limited. We aimed to analyze our lung segmentectomy experience with robot-assisted thoracoscopic surgery.
